Diseases
Click here to view more Diseases
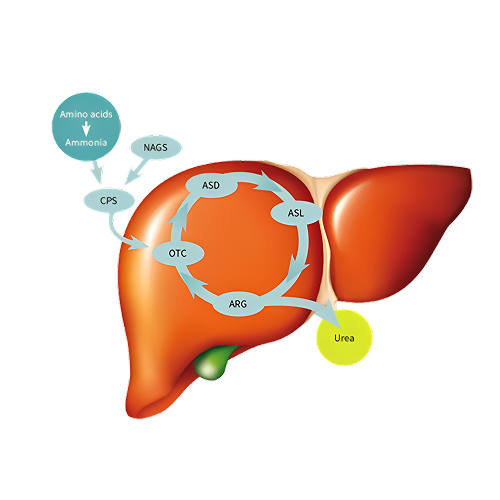
Urea Cycle Disorder (UCD) is a rare genetic condition in which the body cannot properly eliminate ammonia, a waste product formed when proteins are broken down. The urea cycle responsible for removing ammonia through urine is disrupted due to missing or malfunctioning enzymes. Without treatment, elevated ammonia builds up in the blood (hyperammonemia), which can be life-threatening and cause brain damage.
Symptoms of UCD can vary depending on the severity and age of onset. Common symptoms include:
Diagnosis involves a combination of:



